Homelessness is a multifaceted problem that requires a combination of housing, health care and community-based solutions. In this post, we provide a summary of the key insights from our recently published article on health care for people experiencing homelessness, and discuss the need to address intersecting health and social issues through interdisciplinary collaborations between health systems and social services. Our article synthesized research and experience from clinicians, researchers, and service providers over several decades to provide a state-of-the-art overview that is accessible to a wide audience. More specifically, our article highlights homelessness and health, challenges in homeless health care, current approaches in homeless health care, and next steps for homeless health care.
1. Homelessness and Health
Levels of morbidity and mortality are significantly higher among the homeless population compared to the general population. The upstream causes of poor health in the homeless population include extreme poverty, trauma throughout the life course, harsh living environments, and structural barriers to care. The downstream causes include heart disease, respiratory conditions, mental illness, and substance use disorders. Over the past few decades, the downstream causes of mortality have shifted among the homeless population. From the late 1900s to the early 2000s, deaths due to drug overdoses, substance use disorders, and suicides increased, while deaths due to HIV/AIDS and liver diseases decreased.
2. Challenges in Homeless Health Care
People experiencing homelessness face structural barriers, competing priorities, and discrimination that limit access to health care. Primary care providers are well-positioned to provide care for this population by identifying social contributors to poor health and connecting patients to tailored supports. However, many people experiencing homelessness lack a regular primary care provider and rely instead on sources of acute health care. Rates of hospitalizations and emergency department visits are much higher among the homeless population compared to the general population. Re-admission rates are also much higher among this population given poor discharge planning and continuity of care. Finally, recent evidence suggests that the quality of health care provided to the homeless population is worse than what is provided to the general population. Homeless adults hospitalized for cardiovascular conditions in 3 U.S states were much less likely to receive necessary diagnostic and therapeutic procedures.
3. Approaches in Homeless Health Care
Health, health care, and housing are inextricably linked. All people experiencing homelessness should be connected to services that assist with obtaining adequate housing – including permanent supportive housing for those with high needs. Other services such as case management, community mental health programs, and harm reduction programs should also be considered when necessary. Many of these interventions are known to be cost-effective given savings in other medical and social services.
4. Next Steps in Homeless Health Care
Primary care and community-based service providers must work collaboratively to deliver trauma-informed and person-centered care to people experiencing homelessness. Health care systems must facilitate continuity of care, increase access to primary care and community-based service providers, and improve the quality of health care for this population. Housing is central to caring for the homeless population, and the COVID-19 pandemic has shown that homelessness is indeed solvable with enough political will. However, housing alone is insufficient. Homelessness is a multifaceted problem that requires a combination of housing, health care and community-based solutions.
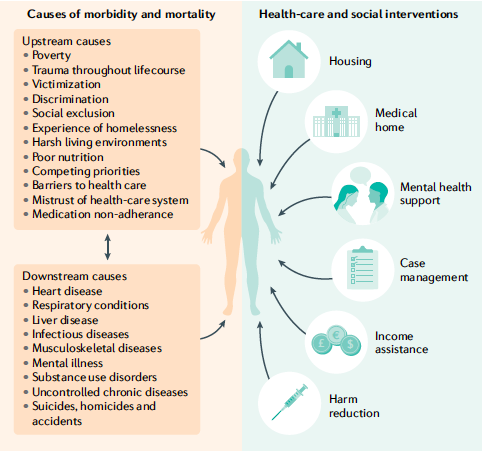
The main takeaway of our article is that people experiencing homelessness face tremendous upstream social burdens and structural barriers that contribute to poor health downstream (and vice-versa). Therefore, health care for this population must address these intersecting health and social issues through interdisciplinary collaborations between health systems and social services.
The analysis and interpretations contained in this blog post are those of the individual contributors and do not necessarily represent the views of the Canadian Observatory on Homelessness.


