People who experience criminalization have the highest rates of hepatitis C virus (HCV) infection in Canada. Even though HCV can now be cured within 8-12 weeks using tablets with almost no side-effects, and testing for HCV has increased substantially in recent years, treatment remains inaccessible to many. From unstable housing to stigma, and poverty to the “digital divide” widened during COVID-19, people experience many barriers to HCV care.
During COVID-19, most services shifted to telehealth or virtual care only. For people without access to the internet or a phone, health care became more difficult to access since the onset of the pandemic.
To improve HCV outcomes, the Test, Link, Call Project is working with people who experience criminalization to support their access to HCV care in British Columbia, Canada. This project was developed to respond to the 2016 World Health Organization (WHO) call to eliminate HCV as a public health threat by 2030, which was endorsed by the government of Canada and included in the Framework. In alignment with these goals, the Canadian Network on Hepatitis C created a Hepatitis C Elimination Blueprint which recommends making programs and services more accessible and acceptable to priority populations. People who experience criminalization (including people who use drugs, people who experience unstable housing, and people who experience incarceration), have been identified as priority populations.
What is the Test, Link, Call (TLC) Project?
This peer-based project is a collaboration between the BC Centre for Disease Control (BCCDC), BC Mental Health & Substance Use Services, BC Hepatitis Network, and Unlocking the Gates (UTG) Services Society. Led by Dr. Sofia Bartlett (BCCDC), Deb Schmitz (BC Hepatitis Network), and Pam Young (UTG), this peer-based intervention aims to broaden access to HCV treatment among people who experience criminalization.
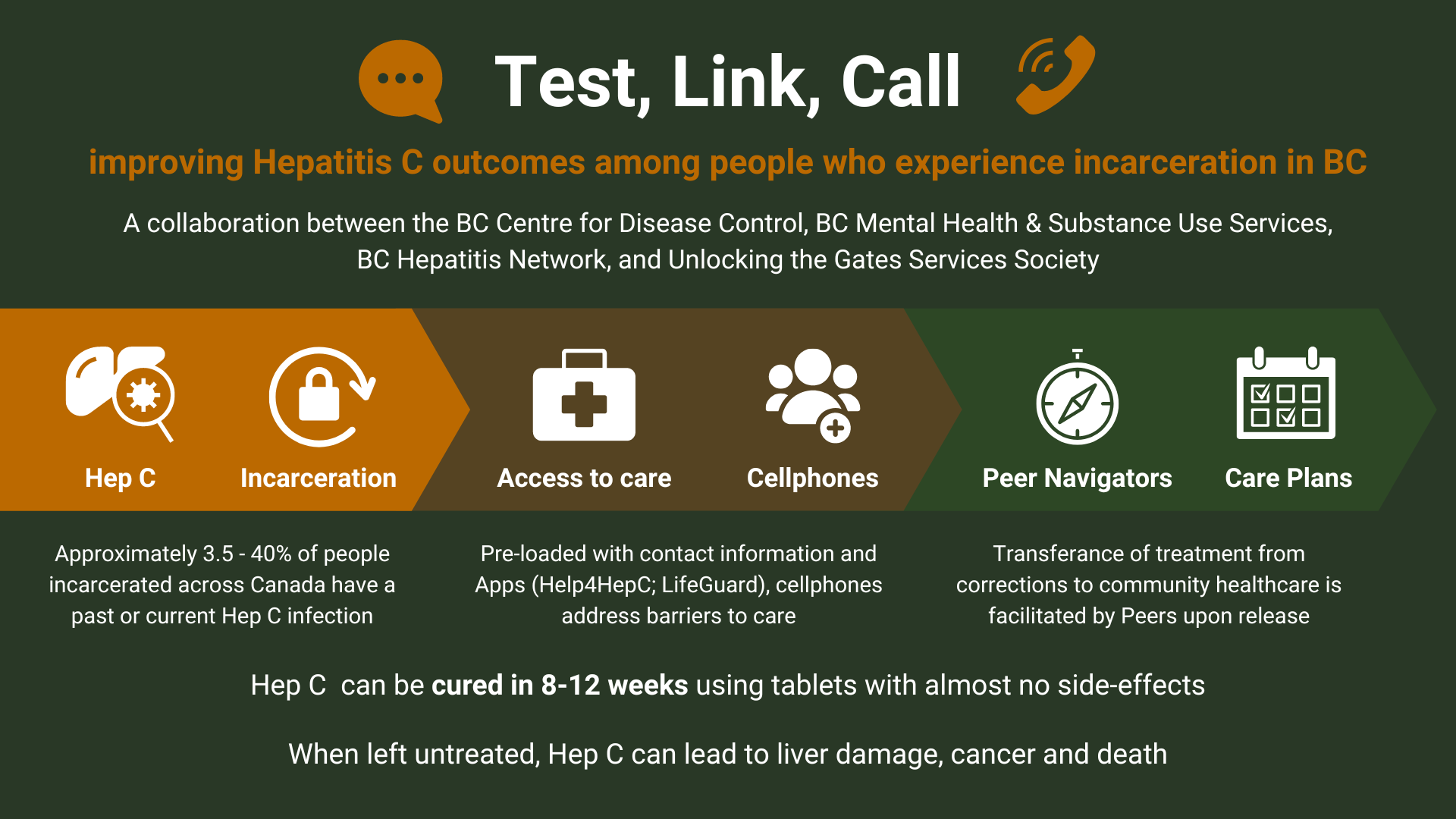
How does the project support access to care?
Project participants are given a free personal cell phone with a 6-month unlimited plan, connected with a Peer Health Navigator, and assisted with appointments for HCV care.
Peer Navigators are staff from the Unlocking the Gates (UTG) Services Society. UTG is a peer-led program that connects people transitioning out from corrections facilities back into their communities with social and health services. The Peer Navigators have been trained in Peers in Practice: Hepatitis C Support by BC Hepatitis Network, and several have also completed further training offered through BCCDC, including the Hepatitis C: The Basics Online Course.
Participants are recruited from shelters, drug detox and recovery houses, and other services by putting up posters with project information in common areas.
Most participants are enrolled after contacting or speaking to a Peer Navigator who explains the project, eligibility criteria, and commitments to them. Health care providers can also refer patients to the project. To enroll and receive a phone, participants must first agree to be tested for HCV or have knowledge of their previous test results. Upon confirmation of HCV infection, their Peer Navigator or healthcare provider will give participants a phone and help connect them to HCV treatment through a network of care providers.
Every phone is pre-loaded with contact information and apps to support the participants’ access to HCV treatment. This includes the number for their healthcare provider, Peer Navigator, and BC Help 4 Hep (toll-free). Additionally, apps include: LifeGuard (harm reduction app), The Brave app (overdose prevention app), MediSafe (medication tracking & reminder app), BC Virtual Visit (telehealth app), BC Services Locator (health service locator app), and I’m Ready (HIV self-test app).
When given their phones, Peer Navigators facilitate the participants’ first contact with their healthcare providers, and determine how they prefer to be checked in with (i.e. call or text) and the frequency of these check-ins. After 6 months, the phones are theirs to keep. However, they are transitioned to a prepaid plan.
How is the project going?
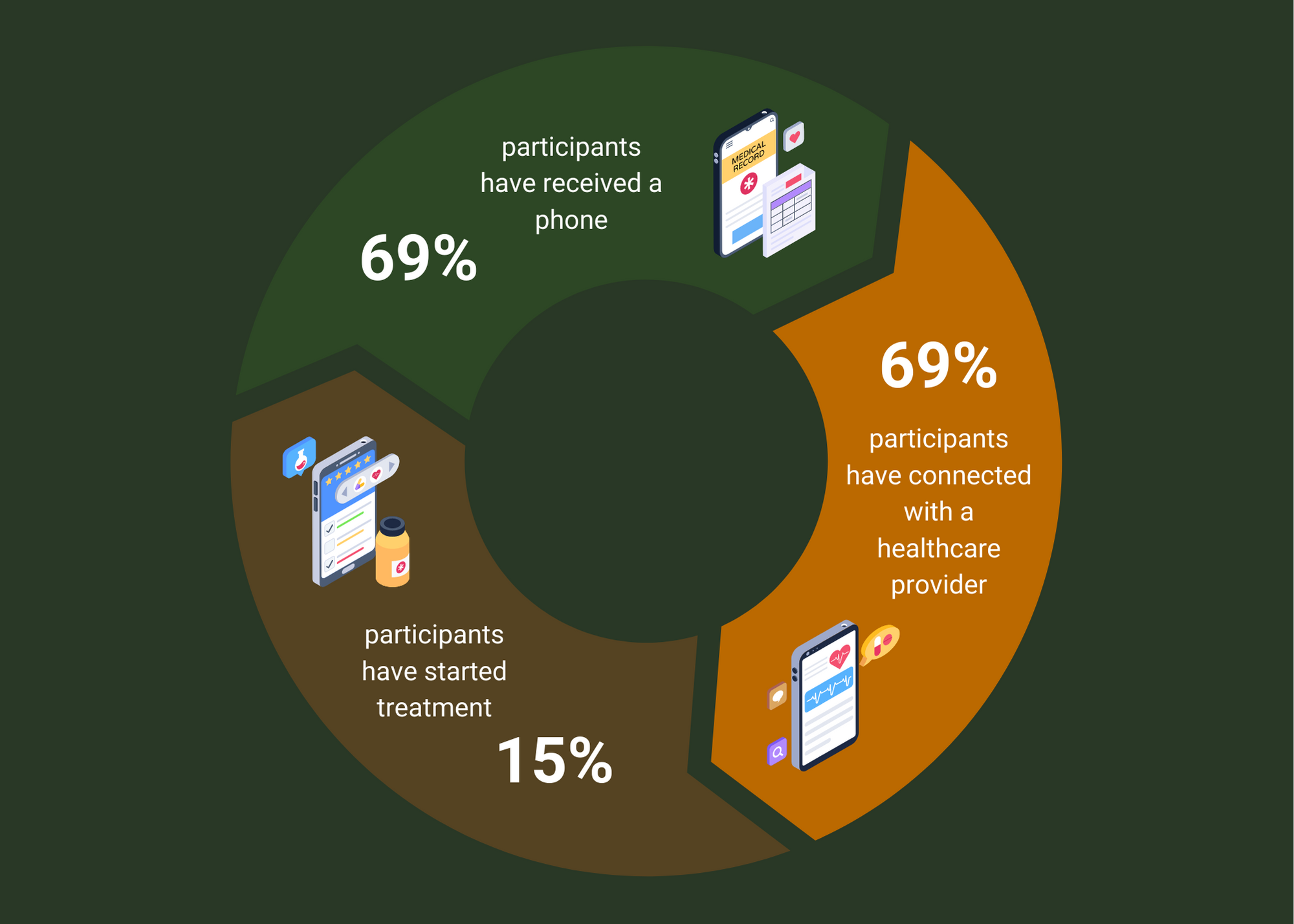
Recruitment began in September 2021 and by our first assessment (March 2022), 13 participants with confirmed HCV infection had been enrolled. Among those 13 participants, 69% (9/13) had received their phone and attended an appointment with an HCV treatment provider, and 18% (2/9) had begun their HCV treatment. There are now 50 participants enrolled in Test, Link, Call and the project will continue to run until the end of 2022.
To improve project engagement, and continuity of care, we are undertaking qualitative interviews with participants and Peer Navigators to understand how their experiences with the project can be better supported.
Want to learn more?
Visit Test, Link, Call Project | YouMatter and/or contact Dr. Sofia Bartlett (sofia.bartlett@bccdc.ca).
Acknowledgements
Thank you to the following groups for supporting participant recruitment and engagement: Unlocking the Gates Services Society, Correctional Health Services Physicians, the HIV and Hepatitis C Specialist Support Team (SST), Regional Chronic Disease Program Northern Health Authority, ASK Wellness Society Kamloops, CoolAid Society Clinic Victoria and Phoenix Society Fraser Valley.
—————-
Meet the Project Team:
Dr. Sofia Bartlett (she/her) is a Senior Scientist for sexually transmitted and blood-borne infections at the BC Centre for Disease Control in Clinical Prevention Services. She has a strong research focus on hepatitis C virus and the health of marginalized populations such as people who use drugs, people who are incarcerated, and people who are unstably housed. Sofia is the Primary Investigator on the Test, Link, Call project. As the Project Lead for TLC, she facilitates HCV treatment referrals with clinics experienced with people who are incarcerated, provides cell phones to the project recruiters and assists recruiters in tracking client treatment progress. Learn more about Sofia and her work at https://stbbipathways.ca/our-team/.
Deb Schmitz (she/her) is the Executive Director at the BC Hepatitis C Network and Collaborator on the Test, Link, Call Project. As a Collaborator, she facilitated Peer Health Mentor’s access to training and supported creation of an online portal that Peer Health Mentors can use to send text messages and reminders to clients’ cell phones through.
Pam Young (she/her) is the Program Manager at Unlocking the Gates (UTG) Services Society. She is the main point of contact for people working with UTG. This includes people leaving corrections, Peer Mentors, and researchers. Pam is a Collaborator on the Test, Link, call Project. As a Collaborator, she facilitates participant recruitment and engagement. Learn more about Pam and her work at https://unlockingthegates.org/.
