People experiencing homelessness (PEH) are significantly impacted during public health emergencies, like the COVID-19 pandemic. Health emergencies of this kind often have health, social and economic impacts on this population. Although PEH or people experiencing housing instability may receive social, housing and health supports through programs like Housing First, they continue to face barriers which make them more vulnerable to the negative effects of health emergencies.
This blog will focus on the findings from a qualitative study that I co-authored. This study aimed to identify the impacts of COVID-19 and associated public health responses on the health, social well-being, and food security of users of Housing First (HF) services in Toronto during the first wave of COVID-19.
Background:
To assess the potential impacts of the COVID-19 pandemic and the strict public health measures implemented on the mental health, socioeconomic well-being, and food security status of HF participants during the first wave of the pandemic (July to October 2020), we interviewed 20 people (10 self-identifying women and 10 self-identifying men) who had accessed the services from one of the three HF programs in Toronto, Canada on a long-term basis. We asked them questions about how the pandemic and response measures impacted their mental health status (either onset of new mental health issues or worsening of existing ones), access to health services, feelings of social connectedness and support, and access to food.
Main findings:
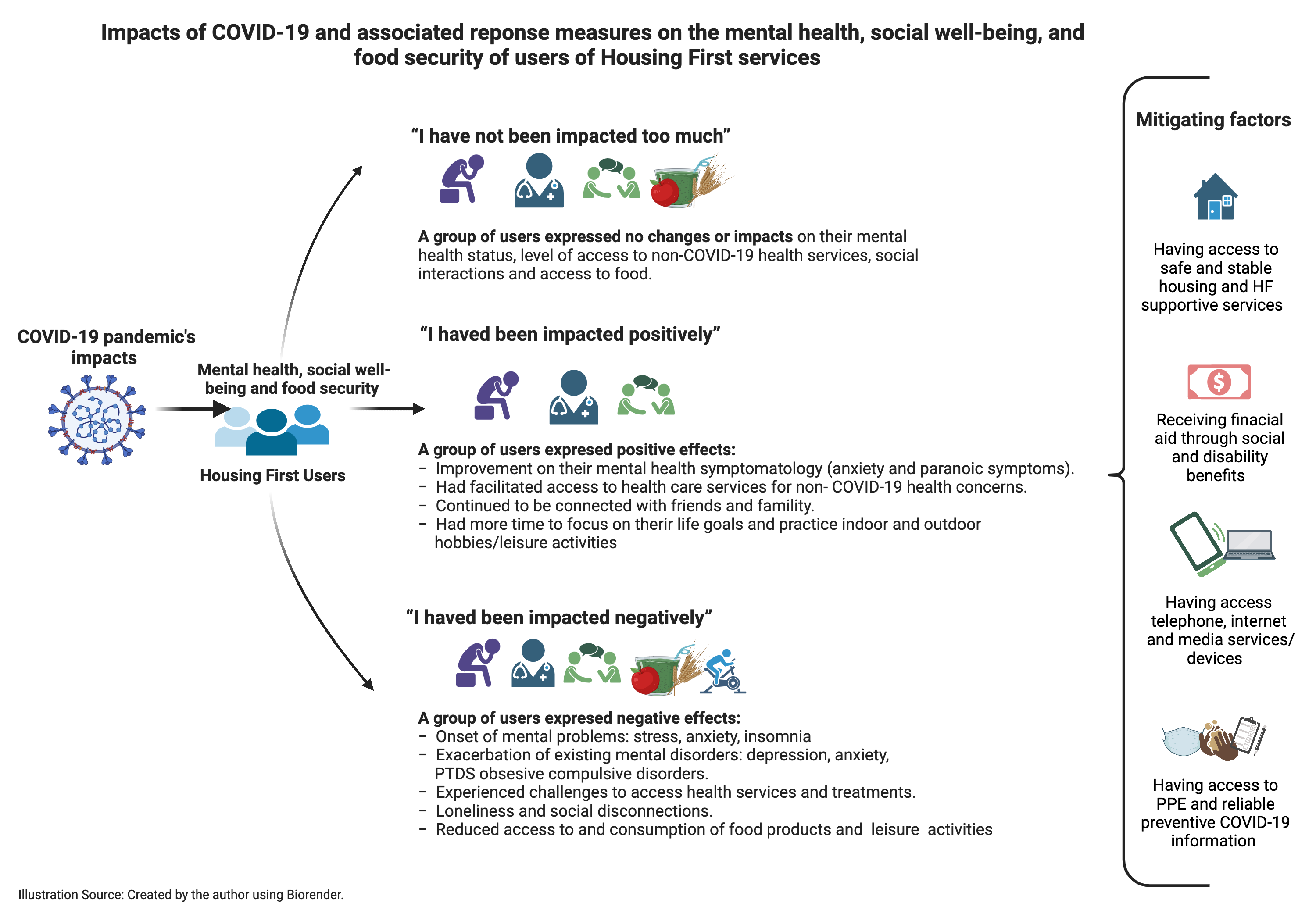 Around 40% of people accessing support from a HF program who were interviewed expressed that the pandemic and associated response measures did not impact or had a minimal impact on their life overall. As reflected by this users’ statements:
Around 40% of people accessing support from a HF program who were interviewed expressed that the pandemic and associated response measures did not impact or had a minimal impact on their life overall. As reflected by this users’ statements:
“I kind of wouldn't say it has. It really hasn't had like that much of an impact [on my mental health]” – Study participant
- Positive impact: For some people accessing services from an HF program, the pandemic and associated response measures brought positive changes to aspects of their life. This included improved mental health status and increased access to health services. In fact, some participants reported a greater focus on seeking help for existing non-COVID-19 related health problems.
“I felt like my mental health… improved because I wasn't always out with people, and having all those little thoughts running through my head all the time about what they think or what are they saying, or all of those ideas that I get” – Study participant
- Negative impact: Among people accessing services from an HF program who reported that they were impacted by the virus, several indicated that their mental health was negatively impacted by COVID-19 and the associated responses. Some experienced new mental health problems (e.g., anxiety, stress, and insomnia). Others reported that their existing mental issues, such as depression, post-traumatic stress disorder, obsessive-compulsive disorder, and anxiety, were exacerbated further during the first month of the pandemic.
“I'm scared, and PTSD-related symptoms started again since the virus showed up for the first time. So, it's quite trying” -Study participant
Also, some participants experienced barriers to accessing continued health care for existing chronic health conditions and associated pharmacological and non-pharmacological treatments. This was a significant challenge. Many participants experienced difficulty in navigating the health system as many health services became virtual. The lack of access to the internet or smart devices and limited appointment availability also acted as a barrier.
“It is not as simple as picking up the phone anymore and making an appointment [with the health provider]. You know, there's usually some waiting involved, so that's frustrating.” -Study participant
Finally, some people participating in the Housing First program experienced loneliness, reduced social connectedness, and were at high risk of food insecurity. Various participants shared that frequent check-ins and the provision of food goods by their HF Case Managers helped alleviate their social and food-related issues.
“Food banks are closed. It has just been a lot rougher. No food access outside the AH [At Home/Chez Soi – Housing First program] program. And food prices have gone up. There are all kinds of stuff that has gone up. Things are not accessible” – Study participant
Conclusion
Based on the results of our study, it is clear that the COVID-19 pandemic had different impacts on the mental health, social well-being, and food security of those accessing the services of a Housing First program during the first months of the COVID-19 pandemic in Toronto, Canada.
The following recommendations were proposed to help strengthen the role of supportive social, health and housing services during public health emergencies in the future:
- Allocate additional financial, technological and personnel resources to Housing First programs. This would mitigate inequities that arise during and beyond public health emergencies significantly. Resources should be tailored to meet the health, social and food needs of HF program participants and other individuals in need who do not have access to such programs or services.
- Provide immediate access to stable and permanent housing, financial assistance, and communication technologies (phone, internet access etc) would reduce exposure to and the spread of the virus among socioeconomically excluded populations.
- Develop and implement person-centred emergency response plans and strategies including:
- Facilitated access to health services
- Sufficient amount of income support
- Continuous child and family supports
- Leisure activities and affordable food.
The full article with findings from this study is available here. To learn more about our research or if you want to connect with the study team, please send an email to the co-principal investigator, Cilia Mejia-Lancheros, at Cilia.Mejia-Lancheros@unityhealth.to

